It's been just over two weeks since the big one; I had my colon removed and was given in its place an ileostomy, which dramatically changes the way I go number two.
As with most stages of my Crohn's journey, I thought I'd write up this blog post with my experiences—and maybe a liiiiittle sarcasm thrown in—for the benefit of anyone else going through a similar situation.
Bowel Prep
My doctor requested a full cleanout for this surgery, I guess so he wouldn't have to deal with stinky poo while yanking out my guts, and I obliged. Unfortunately, for most Crohnies or IBD patients who have to get a colectomy, they're already not in a great place prior to surgery, and neither was I. I was already underweight and not nearly 100% energy-wise, so having to empty out (same prep as for a colonoscopy) meant I did as much as I could to stay hydrated and not faint.
A new step I took during this prep session was the addition of root beer as a chaser to the how-could-anything-ever-taste-worse Suprep I was instructed to chug.

I've also found it important to have as comfortable and stimulating an environment as possible during the purge, so I had my usual bathroom setup.

Some of the things I've always found important while prepping for a Colonoscopy:
- Nalgene bottle full of water; you have to drink at least 32 oz of water after each Suprep dose, so it's good to have a container that helps measure the right amount!
- Table Mate II folding tray table; works great for holding a laptop, iPad, or whatever while you're doing your business.
- RAVpower USB-C 5-port charger — I can keep my laptop, iPad, and iPhone all charged up the whole time I'm prepping! I used to use two separate chargers, but this one is nice for its compactness.
- Small space heater to keep the bathroom a little warm. I find that, even if not dehydrated, the shock to your body of losing a ton of hydration so quickly can give you the chills. Better to combat them with a little heat.
You may also notice some other Crohn's-related amenities I've accumulated for better bathroom experiences, some of which will no longer be necessary with my ostomy: a bidet attachment for my toilet, a squatty potty, and a bath pillow used for frequent sitz baths.
I followed the directions from the surgeon's office, and everyone reacts to Suprep a little differently. For me, I can chug the entire 16 oz mixture in one go, but I have the world's worst tummy ache for about 10 minutes after... then nothing for about 20 minutes... then Niagara Falls for the next two hours. I wouldn't venture more than 20 ft. from the toilet once I start going because sometimes the Suprep-induced urge is that urgent.
My wonderful wife (who has been an amazing companion through all this Crohn's insanity) drove me to the hospital at some crazy hour before the sun was even up. We checked in, and it was a game (as usual) of hurry-up-and-wait, as you wait to be called back, wait for the various docs to check in, wait for the IV, wait for the OR, wait for the operation to begin. The hospital let me wear a comfy 'Bair Paws' gown which spread toasty warm air around my body to keep me warm (apparently this helps prevent complications):

Eventually, the anesthesiologist showed me a vial of happy sleepy juice, and I remember nothing from that point until:
Recovery in the Hospital
Managing the pain
Before a partial resection of my ascending colon in 2016, I never had a major surgery. I came in ill prepared, and only realized how long the recovery would take after I was lying in pain in the hospital bed a few days later.
This time around, I knew to expect more pain, and a long road to recovery, but I didn't quite realize how hard it would be.
Day one, I was cracking a joke or two: my favorite was "when I was in the operating room... they had me in stitches!" My pain receptors were also still pretty knocked out from the lingering anesthesia drugs and some regular doses of morphine.
But day two in recovery, the pain packed a huge punch, and I was writhing in pain. I even remember, for a short time—the only time I've felt this in my life—that I felt alone and like the pain would never stop. This, with my wife sitting to my right and my Mom sitting to my left!
Day three came and the pain subsided a tiny bit. Day four, a little more, etc. Each day I'd need fewer doses of oxycodone to fend off the 5+ levels of pain. (I experienced a few 9s and 10s while recovering from this surgery!)
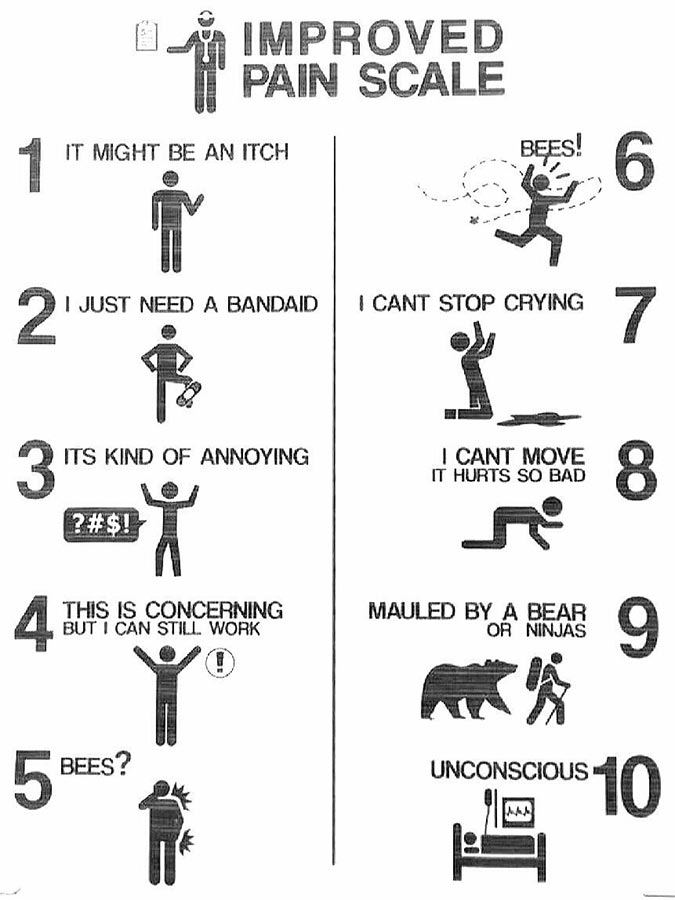
Source: Imgur.
I didn't really know what to expect since I was having some major patching up done internally, on my abdomen, and on my rump! Three separate areas where pain could express itself in new ways, each time I'd move, turn, or gesture. For anyone who decides to do the whole enchilada—a proctocolectomy with ileostomy—just know that it's going to bite like a bulldog, and hang on for a few days. And there is no shame in requesting pain meds when you're experiencing 9s and 10s!
Aside: One other type of pain that you'll never experience outside recovering from a long laparoscopic operation is the pain of extra CO2 gas left over from the operation. The doctor used gas to inflate my belly to give some working space during the operation, and a little bit of that gas remained and migrated to my shoulders afterwards. That stuff, for some reason, hurts like you wouldn't imagine! And nothing—not a shoulder rub, not holding your arm in any position—nothing stops that pain. You just have to keep moving around as much as you can and wait for the gas to dissipate.
PT, OT, they all stand for 'Torture'
Meanwhile, in the midst of trying to manage my pain, these crazy people called 'OTs' and 'PTs' waltzed in and told me I had to start doing things like walk. Or bend my leg. How dare they!

I know in my head it's good to walk and move around as soon as possible post-op... but when your body is screaming DON'T MOVE, it's a lot harder. Fortunately, I was able to muscle through the pain each day and get up on my own two legs a few times. I had a walker, and probably looked like I was 90 years old, hunched over inching along in my yellow grippy socks. But it was something. I kid about Therapists being Torturers, but only slightly. Sadly, someone has to do the job, and amazingly the OTs and PTs I had were all very nice people, despite their patients' hesitance.
Things sticking out of your body
While I'm on the subject of torture, I would be remiss not to mention all the various doodads you'll find hanging out of various body parts:
- An IV in your arm or wrist, feeding some concoction of drugs and IV fluids.
- A secondary IV in your other arm or wrist, because why not?
- A catheter coming out of your privates.
- A 'JP' drain coming out of some part of your stomach.
At least that's what I had. Lots to keep track of, especially every time you want to move, roll, get out of bed, get into bed, or do pretty much anything. And if you forget about one of the many tubes, you end up yanking on some sensitive area or another, and the pain meter spikes back up to at least a 7!
And of course, for every one of the items listed above—most of which were inserted while under sedation—you'll go through the rather unpleasant experience of a doctor or nurse yanking them back out, with zero sedation and full awareness.
Keeping up the spirits
All is not doom and gloom, though. I knew I'd be getting myself into this, and that it will be worth it in the end. To help remind myself of that fact, I had two extremely helpful supports in my recovery room:
- Visitors
- Decorations
Since we had time to plan out my surgery, my wife and I were able to line up a babysitter so she could come to the hospital every day. Having her there to support me, talk to me, and just sit next to me (whether or not we were talking) was a huge blessing. It can get really lonely sometimes, when nobody's around and it's 3 hours until the tech comes back in for vital signs. Having someone there from time to time cancels out that loneliness.
Every once in a while, things can be a little awkward (e.g. when you're clambering out of bed and all your hoses are showing all your bodily fluids—blood, urine, and stool!), or you can feel like you're being a burden to someone visiting. But worst case you can ask the visitor to go out into the waiting room, or grab a meal at the cafeteria (my treat!).
Between my wife, my sister, my Mom and Dad, my aunt and uncle, and a couple friends, I had someone besides nursing staff to talk to much of the day. Very nice when holding up my phone or Kindle for more than ten minutes was a burden!
Speaking of my sister, I remember a couple decades ago, when she was born, I would come and visit her in the hospital daily—she was born three months premature and I was her big brother, so I had to keep watch over her while she grew strong enough to go home!

Now more than 20 years later, I was honored by her presence while I was in the midst of the worst pain I've ever experienced. She got the chance to help me grow strong enough to return home to my family. ?

My wife and children also spent some time pre-op drawing pictures and making little decorations to hang around my room. During the most intense moments of pain, being able to focus on one of these little tokens of love from my 1, 3, and 5 year old, hung just so around the room by my wife—this was a major source of consolation. It kept me grounded and gave me a reason to remember why my suffering will be worth it in the end.
Although, I will admit, every once in a while, the irony of waking up in the middle of some head-splitting pain and seeing a giant "YAY" right in front of my face was not quite as humorous as I'd thought when I bought the inflatable sign at Target:

A lowercase 'yay' is about all I could muster, too, whenever I realized I'd have to start managing 'the bag' that is part and parcel to having an ostomy (and becoming an "ostomate").
Getting 'The Bag'
"This is a Hollister bag."
— My WOC nurse
Oh cool, who knew Hollister was so into helping patients with ostomies? You wouldn't think they are dedicated to poop-catching bags, right? Will I leave the hospital looking a bit like this?

I wouldn't mind having my abs a little tighter, chest a little more ripped...
Oh, wait, you mean there's another Hollister? Oh. This one doesn't make fashionable clothing and accessories, but rather a bunch of sterile-looking hospital-colored plastic baggies that people stick on themselves:

Well. That's nice. So let's get this straight:
- I have a new squishy bump on my belly.
- It's constantly flatulating of its own accord.
- It's constantly pumping out poo of its own accord.
- I have a crazy-sticky bag attached that catches said poo and gas.
- The bag is from Hollister, but not the 'cool' Hollister... the Hollister associated with icky bodily waste collection.
Wonderful. This just keeps getting better!
Sarcasm aside, the bag is a great blessing for me; I didn't sit on the toilet one time while I was in the hospital. In fact, the only time I've sat down on a toilet since surgery day was to change my bag at home, which only took about 10 minutes. So far I've saved a few dozen hours of my life not sitting on the toilet due to Crohn's!
Having to wear and maintain an awkward medical device beats not having any time to be with my family and enjoy life, so ? from me!
Going Home
I find recovering from a major surgery has a few high and low points. Unfortunately for those who help at home, the first day/night at home is a definite low point. At the hospital, even though it's overall a jarring experience, my body was getting used to the bed, the eating position, the every-four-hour vital signs, the assistance of nurses and techs, etc.

When you go home, you not only have to deal with a bumpy, turn-y car ride (oh so painful after abdominal surgery, and doubly so if you have active wounds all up your hindquarters!), you also have to go back to a place where you know it should be more comfortable and, well, homey, but it's not:
- Your bed is flat. This makes sleep very... weird. And in my case, sweaty and difficult to sustain the first few nights.
- You have to walk to the bathroom any time you need to do anything since there are no techs to help empty all your waste-collection devices.
- You have all your home comforts and pastimes to tempt you, but you're in no shape to be able to do your usual routines.
Sounds like some real #firstworldproblems... but they're not, really. It's a strange experience coming home when your body is radically different, and still in a pretty fragile state.
One of the strangest feelings that I don't think you can feel unless you've had abdominal surgery is the 'gut spilling out' feeling. Maybe it's just me, but whenever I lay on my side the first few weeks after surgery, it feels like all my intestines are slowly squishing over onto that side, and could very easily spill right out of my gut!
It feels like there's a big ball of wet spaghetti inside my belly, and it shifts when I shift. So side-sleeping is out, for now. Luckily I found this handy wedge pillow from Bed Bath & Beyond to make back sleeping almost as comfortable as in the hospital bed. On sale and with one of those 20% off coupons, the price isn't too steep.
I also considered renting a cane or walker for the first few days, but thankfully it didn't become necessary. I could just hobble around like a turtle for a few days until my back was able to straighten a bit.
After returning home and hitting the low point of the first day and night, you soon hit another high, where you start to feel like you'll be able to do anything you used to be able to do soon! And for me, that meant going downstairs and replacing an air filter in the furnace. Bad idea. Body's not ready for it yet, dummy!
So then you have another low the next day, as your body recovers from your overachieving choices the day prior. But as the healing progresses, and you feel a little better each day, it's not so bad. I'm able to sit almost fully upright for a short meal after two weeks. I can type a little bit before fatiguing.
Summary
There is still much for me to learn about my new friend, the stoma. I haven't named mine (many people do). I have learned that there are about 3,000 different pouching systems to look into, hundreds of pouch accessories, different philosophies for keeping things clean, wearing ostomy bags, bathing, swimming, etc. It can be overwhelming, but one great comfort is that I've so far never had a leak—apparently a lot of ostomates (those who have ostomies) have problems with that.
The next major challenge: finding a way to sit in a car with a seatbelt with an ileostomy! I imagine my next Crohn's-related blog post will discuss the ongoing adventures of living with a poop-volcano stoma!
Comments
You're back!! YAY!! (no lowercase stuff here.) Well, I'm happy to share with you that one of my most favorite things in life is when I get to change "please, God" to "thank you, God." And, while your humor is inspiring, I know you've been through an ordeal. But, having endured it now, going forward I'll just offer best wishes that it's all down hill from here. So, while you were gone I built a Drupal PI!! And, other than a couple of minor blips which I was able to work through myself, it worked perfectly!! I built the project with Ansible onboard the PI so my next effort will be to install Ansible on my Linux PC, and re-run the project to build the Drupal PI remotely. Plus, the price of the Raspberry PI 3 B+ dropped a couple of bucks today on Amazon, so given a successful remote install, I think it's time to jump on the PI Dramble!! I'll let you know how it goes. Standby for some humor. ;) Once again, welcome back!!
Thank you for sharing this, Jeff. Take your time and get strong. We love you!
Man, great that you share this typical unseen operations. Hope you and your new friend can get along well in the future!
Jeff - very brave and selfless of you to share this. Our thoughts and prayers are with you.
Glad you are back. I must say you are brave.
A very well written and relatable piece that gives comfort to many and helps us all to better understand the struggle. You are awesome for having shared this. I perforated my colon last year around Christmas and so much of what you wrote here rang true for me as well. It was truly great of you to share this journey with us and I wish you the best in your recovery and your ongoing situation with Crohn's.
Hi, I'm one of those random internet strangers. I came in off your Github profile and was curious to know more about you. I was not disappointed :)
As you undergo your journey in learning how to live this new life of yours, don't be afraid to experiment with things that might seem unconventional. Look up Todd Stabelfeldt ( a.k.a, "The Quadfather" ). This guy was looking at using RV parts to help with his mobility issues as a lot of the assistive devices he was finding were of poor quality.
His situation is nowhere near the same as yours but it's a wide open world out there.
Thanks for sharing. Feel better.
Reading your post was so comforting as I am also recovering from a major Crohn’s surgery. Thank you so much for sharing.
Just got a stoma. Here two weeks post op and so many problems. 5 liters a day and trying to reduce. This is tough.
Praying for you; the first couple weeks are a doozy, I hope you are getting the support you need! Make sure you find a good WOCN to help too, and if you can find others who you can talk to, e.g. through UOAA support groups.
Wow that was beautiful ! Thank you so much for sharing your experience. I’m 10days post op for a tear in my large intestine/ sigmoid colon, consequences of 20 years of Crohn’s disease. Iv only been home for 3 days and I ran across your post after searching google for “intense stomach pressure after surgery” and I’m so glad I did. I have this bag hanging off my body, an 8 inch long open surgical wound on my stomach and a painful hole where the jp was. Everything is so weird now I don’t really know like what to do or if I should do anything at all. Haven’t really slept well in the whole 10 days, I wake up in shock and drenched in sweat after 2 or 3 hours of falling out. I’m falling asleep while I’m writing this so I just wanted to say thank you, Your story was exactly what I needed to read. So beautiful .
Good luck! If it's any consolation, I'm a year out and still have some trouble sleeping here and there. It's a long slow process to find your new normal. It took me at least two months before it felt like I could sleep without my insides coming out (I knew they wouldn't, but it felt like jello in there!).
Just been thru the same surgery. Colon and rectum removed due to UC. Thanks for sharing your story... Very encouraged. I'm home for a week now and just shuffling thru my days.
Shuffling through days is an accurate description of the first couple weeks. I was so bored after a few days at home, especially since it took more effort to even watch a video on my iPad than it was worth!
After a couple weeks I had the energy to watch a movie but not read a book, so I wound up watching about 40 movies and 2 TV series that week. Then I could read again, so I went through a few books I'd had on my 'to read' shelf a while :D
Thank you! ????
Thank you for sharing. I will be having my colon removed in a couple of weeks and it is good to have insight into what to expect. Here's to a new "normal."
Best of luck!
Did you feel worse around week 3? I
Seems like I’m feeling more discomfort maybe as things heal. When did you feel normal ?